Vaginectomy: Critical Info for Trans Men
Vaginectomy is a surgical procedure that removes the vaginal lining and closes the vagina. Many transgender men have a Vaginectomy combined with other FTM surgeries as part of their gender confirmation. Vaginectomy has had a reputation for being a very risky procedure but surgeons specializing in it believe that Vaginectomy reduces complications associated with urethral lengthening, and report high rates of satisfaction among patients.
In the context of FTM surgery, Vaginectomy is a Colpectomy plus a Colpocleisis. Colpectomy involves removal of the vaginal lining, or epithelium, and Colpocleisis is the fusion of the vaginal walls, which creates support for pelvic organs. Most commonly, the general term Vaginectomy is used instead of Colpectomy and Colpocleisis. Finally, some surgeons offer partial closure of the vaginal opening in combination with Simple Release and Ring Metoidioplasty but this is not to be confused with Vaginectomy; it is just partial closure.
Is Vaginectomy Really That Risky?
For many years, Vaginectomy endured a reputation for being a very risky procedure—so risky, that many surgeons refused to perform it and even discouraged trans men from seeking it out, citing major intraoperative bleeding and bladder perforation as high risks. While there is very little published data regarding the safety of FTM Vaginectomy, recent reports from surgeons experienced with the procedure indicate that with modern techniques Vaginectomy may not be as risky as previously thought, and may even reduce complications associated with urethral extension.
Dr. Burt Webb, one of the most experienced surgeons in the United States when it comes to FTM gynecological surgery, has perfected his Vaginectomy technique to minimize blood loss. He has also noted very low complications rates in patients who had Vaginectomy combined with lower surgeries that included Urethroplasty. By eliminating vaginal secretions and improving blood flow to the urethra by fusing the vaginal walls, the surgical sites—especially the critical urethral junction—heal better.
"A normal complication rate when [Vaginectomy] is not done is roughly 40-45% ...the complication rate when a Vaginectomy is performed with these procedures is less than 3%."
Source: ftmdoctor.com
Urologist and Plastic Surgeon Dr. Curtis Crane described complication rates of at least 25% when Vaginectomy is not performed alongside Urethroplasty, reducing to 10-20% when it is performed.
The gender surgery team at VU University medical center, Amsterdam, Netherlands has made Vaginectomy a standard procedure prior to Phalloplasty and Metoidioplasty with urethral lengthening because they believe it reduces fistula rates.
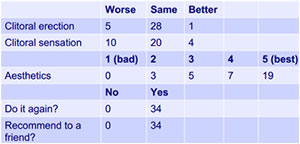
Surgeons at the Institute of Urology London reported that complications with Vaginectomy are few and easy to manage, and that the amount of bleeding is directly related to vaginal length. Additionally, they reported a high satisfaction rate among patients.
4 Reasons Why Trans Men Have Vaginectomy
- The desire to have the vagina removed and have a male-looking perineum.
- To eliminate the secretions produced by vaginal mucosa.
- To eliminate the need for speculum exams or Pap tests.
- To reduce complications with Urethroplasty.
How Vaginectomy Is Performed
- Incisions are made inside the vagina and the vaginal mucosa is carefully removed by excision or ablation.
- The vaginal walls are sutured together and the vaginal opening is closed.
- Operative time is 2-3 hours.
- Laparoscopic and robot-assisted laparoscopic Vaginectomy are emerging methods.
Vaginectomy is usually combined with other procedures, either Hysterectomy or a genital surgery. There are many benefits to combining Vaginectomy with other FTM surgeries, such as lowering the risk of complications with Urethroplasty, as well as reducing costs and time off work, and no additional recovery time.
Some surgeons require a Vaginectomy for patients undergoing Metoidioplasty or Phalloplasty, especially if Urethroplasty is performed, because of the theory that Vaginectomy reduces complications associated with the neourethra.
When indicated, Vaginectomy can be performed as a standalone procedure, though Urologist Dr. Maurice Garcia recommends Primary Urethroplasty (a repositioning of the urethral opening) when getting a Vaginectomy to reduce the risk of urinary infections.
Hysterectomy is required for all patients having Vaginectomy.
Vaginectomy and Recovery
Length of hospital stay, recovery time and time off work all depend on if Vaginectomy was combined with other procedures or not. Similarly, restrictions on prolonged sitting, cycling, swimming, hot tubbing, heavy lifting, and sexual activities will vary based on the procedures done.
Patients will experience some pain but this typically diminishes significantly within two weeks. Longer term discomfort is not uncommon with prolonged sitting and activities such as cycling and horseback riding.
 This article was expert reviewed by Dr. Burt Webb, MD. Dr. Webb is one of the most recognized OB/GYN's in Arizona, as well as one of the most experienced surgeons in the United States when it comes to FTM gynecological surgery. His dedication to reducing complications with Hysterectomy and Vaginectomy have made him the go-to Gynecologist for trans men in the U.S.
This article was expert reviewed by Dr. Burt Webb, MD. Dr. Webb is one of the most recognized OB/GYN's in Arizona, as well as one of the most experienced surgeons in the United States when it comes to FTM gynecological surgery. His dedication to reducing complications with Hysterectomy and Vaginectomy have made him the go-to Gynecologist for trans men in the U.S.
Vaginectomy Journal Articles
Robot-assisted laparoscopic colpectomy in female-to-male transgender patients; technique and outcomes of a prospective cohort study [Full text]
Freek Groenman, Charlotte Nikkels, Judith Huirne, Mick van Trotsenburg, Hans Trum
Surgical Endoscopy, August 2017, Volume 31, Issue 8, pp 3363–3369.
Study results show that [robot-assisted laparoscopic Vaginectomy] combined with [robot-assisted laparoscopic Hysterectomy] is feasible as a single-step surgical procedure in FtM transgender surgery.
Laparoscopic Vaginal-Assisted Hysterectomy With Complete Vaginectomy for Female-To-Male Genital Reassignment Surgery.
Gomes da Costa, Valentim-Lourenço, Santos-Ribeiro, Carvalho Afonso, Henriques, Ribeirinho, Décio Ferreira. J Minim Invasive Gynecol. 2016 Mar-Apr;23(3):404-9.
This study suggests the feasibility of laparoscopic vaginectomy in genital reassignment surgery. The procedure can be executed as a continuation of the hysterectomy with the potential advantage of the laparoscopy providing better exposure of the anatomic structures with low blood losses (less than 500 mL) and few complications. Furthermore, using this approach, adequate-sized vaginal mucosa flaps were obtained for the urethral reconstruction.
Outcome and Risk Factors for Vaginectomy in Female to Male Transsexuals
M. Spilotros, DJ Ralph, N Christopher, Institute of Urology London, presented at the World Meeting on Sexual Medicine. 2013.
This presentation includes reasons, treatment and results for vaginectomy. Complications are few and easy to manage. The severity of bleeding is directly related to vaginal length. Patients report high satisfaction rates.