Hysterectomy Risks & Complications
As with any surgery, there are both short term and long term risks associated with having a hysterectomy. Although hysterectomy is a frequently performed procedure, it should not be underestimated in terms of the potential for complications.
A 2010 study queried participants about the complications they experienced after hysterectomy:
- 25% Experienced post-surgical onset bladder/urinary problems. The most common bladder/urinary problems included increased urinary frequency (14%) and frequent/chronic pain during urination (5%).
- Keloid scarring (10%)
 Infections (8%)
Infections (8%)
- Adhesions(6%)
- Post-surgical bleeding (3%)
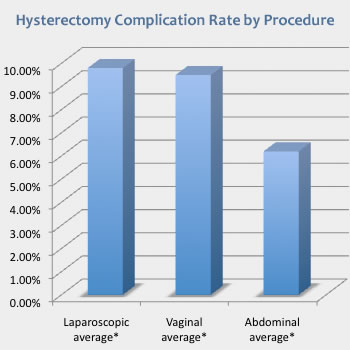
The 2004 eVALuate study compared complication rates between TLH, LAVH and Abdominal Hysterectomy:
Laparoscopic hysterectomy was associated with a significantly higher rate of major complications than abdominal hysterectomy. It also took longer to perform but was associated with less pain, quicker recovery, and better short term quality of life. The trial comparing vaginal hysterectomy with laparoscopic hysterectomy was underpowered and is inconclusive on the rate of major complications; however, vaginal hysterectomy took less time. Source: The eVALuate study
Short Term Risks of Hysterectomy
Adverse reactions: Nausea and vomiting, breathing or heart problems due to anesthesia.
Pain from CO2 gas: At the beginning of surgery, your abdomen is filled with gas to give the surgeon adequate internal visibility of your organs. The CO2 gas can become trapped against the diaphragm causing organ, diaphragm and possibly shoulder pain.
Infection: Wound infection or infection of the bladder, chest, or abdomen may necessitate antibiotic treatment.
Urinary problems: Kidney, bladder and/or urinary tract infection; temporary urinary incontinence or retention, requiring continued use of a catheter.
Hemorrhage: Excessive blood loss during or after surgery which requires blood transfusion.
Blood clots: Can happen in the veins in the leg (Deep vein thrombosis aka DVT) or pelvis. The risk is increased by smoking, inactivity, excess weight and oral contraceptives.
Adjacent organ perforation: Rectal fistula, vesicovaginal fistula or urethral fistula are serious complications that involve an abnormal connection between two spaces and fecal and/or urinary incontinence.
Long Term Risks of Hysterectomy
Urinary Frequency or Incontinence: Can be caused by accidental damage to the pelvic nerves.
Menopausal symptoms: Hot flashes, sleep disturbance, headaches, etc. can occur in trans men, even if the ovaries are left in place (due to decreased blood flow to the ovaries after hysterectomy.)
Reduced sexual satisfaction: In a 2010 study, 6% said that sexual response was worse after hysterectomy.
Prolapse: After hysterectomy, the intestines, bladder and vagina are no longer supported by the endopelvic fascia and can drop, leading to constipation and/or urinary incontinence/inability to control bladder and pain during sex. The risk of prolapse is heightened in those who have given birth, as the pelvic floor muscles are weakened.
Autoimmune disorders: There's little research to rely on, but anecdotal reports about the onset or worsening of autoimmune disorders after hysterectomy are common. (On the flip side, there are also anecdotal reports of improvements in autoimmune disorders post-hysterectomy.)
Adhesions: Internal scar tissue can attach itself to organs and cause pain and other problems.